End-to-End Revenue Cycle Support for Healthcare Providers

Our Experience in Numbers





Our Revenue Cycle Management Services Include
Patient Demographics & Charge Entry
- Accurate patient demographic verification
- Charge entry and validation
- CPT, ICD-10, and HCPCS review support
Medical Coding & Claim Submission
- Coding accuracy checks
- Clean claim preparation
- Electronic claim submission to Medicare, Medicaid, and commercial payers
Payment Posting Services
- ERA/EOB review and posting
- Insurance and patient payment posting
- Adjustment posting and reconciliation
- Identification of underpayments and discrepancies
Who Our RCM Services Are Designed For
- Independent medical practices
- Specialty clinics
- Hospital-based providers
- Hospitals and nursing care centers
- Medical billing companies seeking operational support
We customize our RCM engagement based on practice size, specialty, claim volume, and workflow preferences.
Accounts Receivable (A/R) Follow-Up
- Timely follow-ups on unpaid and underpaid claims
- Payer-specific investigation and resolution
- Appeals and reconsiderations
- Aged A/R cleanup (30/60/90+ days)
Denial Management & Appeals
- Root cause analysis of denials
- Corrective action implementation
- Appeal preparation and submission
- Denial trend tracking and reporting
Revenue Reporting & Analytics
- Daily, weekly, and monthly billing reports
- A/R aging reports
- Collection performance metrics
- Custom reporting based on client needs
Compliance & Quality Assurance
- HIPAA-compliant workflows
- Internal quality checks
- Continuous process improvement to reduce errors and denials
Why Outsource Revenue Cycle Management to Us?
- Improved cash flow and faster reimbursements
- Reduced claim denials and rework
- Lower administrative overhead
- Transparent reporting and communication
- Scalable support as your practice grows
Whom do we serve?
- Independent Medical Practices
- Multi-Specialty Clinics
- Mental Health & Behavioral Health Providers
- Medical Billing Companies
- Healthcare Startups & Growing Practices
We tailor our services to your specialty, volume, and growth stage.
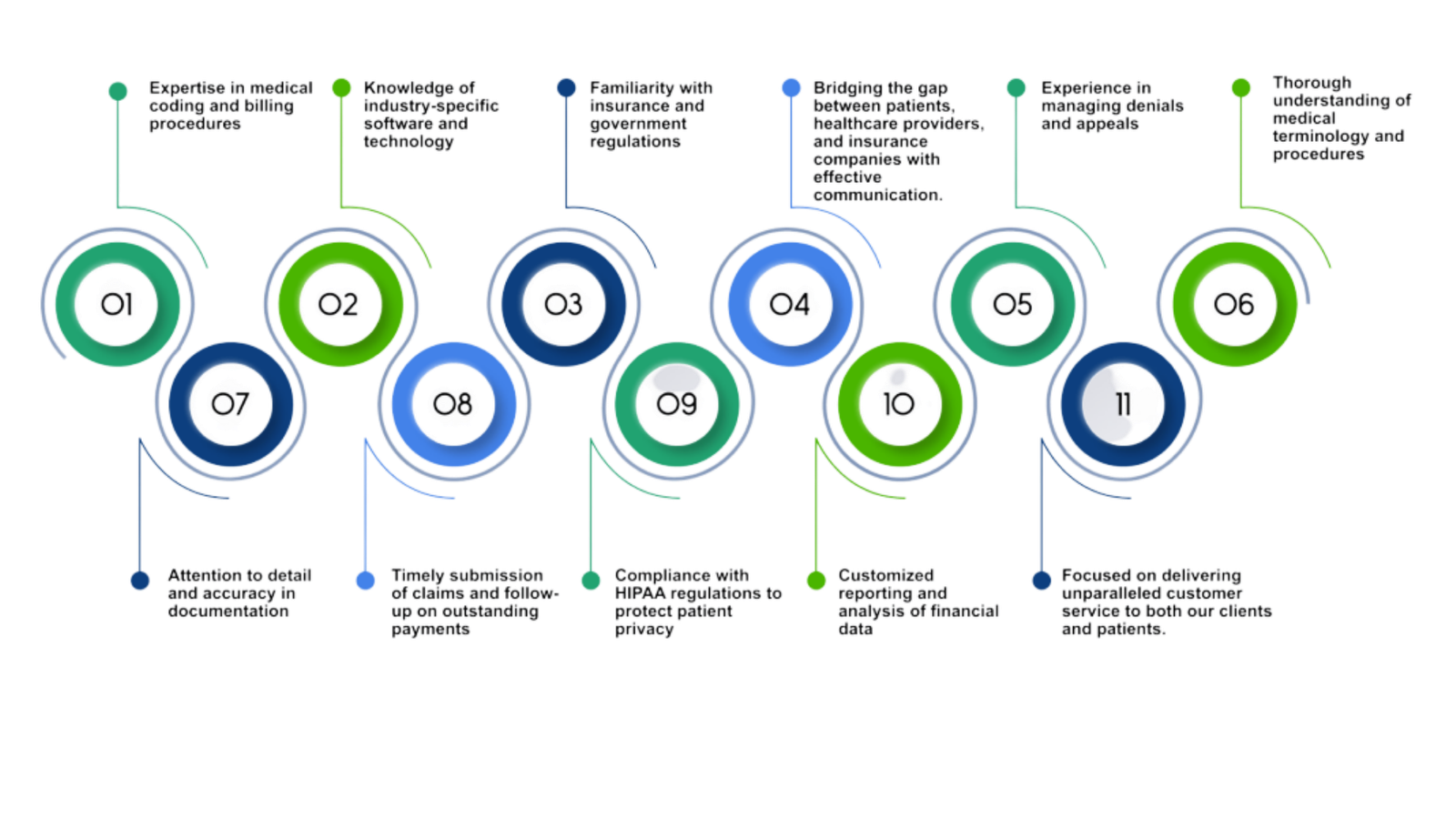
What makes Amogh Medical Management USA one of the best medical billing Company
Leverage Our Expertise to Stay Ahead of the Curve
Optimize Your Results with Our Streamlined Process
Navigating the world of medical claims billing can be a real headache. But don’t worry – our AMM’s medical billing services got you covered! You’ll be on your way to financial success with eight simple steps.

Patient's Demographic Entry
Our team makes creating a new patient account by collecting demographic information from healthcare providers a breeze. Our skilled and experienced staff use electronic resources to maintain standard operating procedures, which helps prevent errors.
Insurance
Verification
At HMS, our billing experts kickstart the insurance verification process by contacting the patient’s healthcare insurance provider through phone or email. They check if the patient has an active health insurance plan and is up to date with the premium payments.
Medical Billing and Coding Services
At HMS, we’re experts in converting medical conditions and procedures into the appropriate ICD codes and healthcare services into CPT codes using advanced coding software. Plus, we’re certified by AAPC as a practice revenue manager
Charge Entry
Our HMS medical billing and coding services handle the tedious task of charge entry so you can focus on what matters most. We will also ensure that the payment made by the patient at the time of their visit is recorded in your system.
Claim Generation
Our medical billers make the claim submission process simple and easy for you. They gather all the information from the encounter form and prepare and submit the claim to the patient’s insurance company.
Claim Scrubbing
We take extra precautions to ensure that every claim is error-free. Our medical billing services include claims scrubbing software to check and correct any mistakes.
Claim Tracking
At HMS, we take the hassle out of medical billing by keeping you informed every step of the way. Once we submit your claim, our billing department watches its progress, using cutting-edge technology to get frequent status updates.
Denial Management
Don’t worry if your claim is denied; our experienced staff knows how to handle it. We get remittance advice with a denial code and explanation, and our billers review the claim to see where we can improve. We’ll add any missing information and make sure the claim is corrected.
A/R Collections
Our medical billing services at HMS continues beyond clearing claims and receiving payments. Our dedicated AR Team continuously work on claims to get them paid.
Schedule Your Free Consultation Today
